Osteoporosis: What is it and why should I care?
Prevalence
Osteoporosis Australia estimate that in 2022, 6.2million Australians over 50 have osteoporosis, osteopenia, or poor bone health, which is 66% of all Australians over 50. Of these people, 22% have osteoporosis and 78% have osteopenia. It is estimated that 29% of health system expenditure on falls can be attributed to low bone density (Australian institute of Health and Wellness, 2023), and that osteoporosis and osteopenia cost the Australian healthcare system $2.75 billion annually. Though osteoporosis is thought to be something that primarily affects women, this is not to say that men are completely unaffected: men account for approximately 30% of osteoporotic fractures recorded.
What is osteoporosis/osteopenia?
Both of these conditions are diagnoses that are made based on your bone density, which is determined through a DEXA scan.
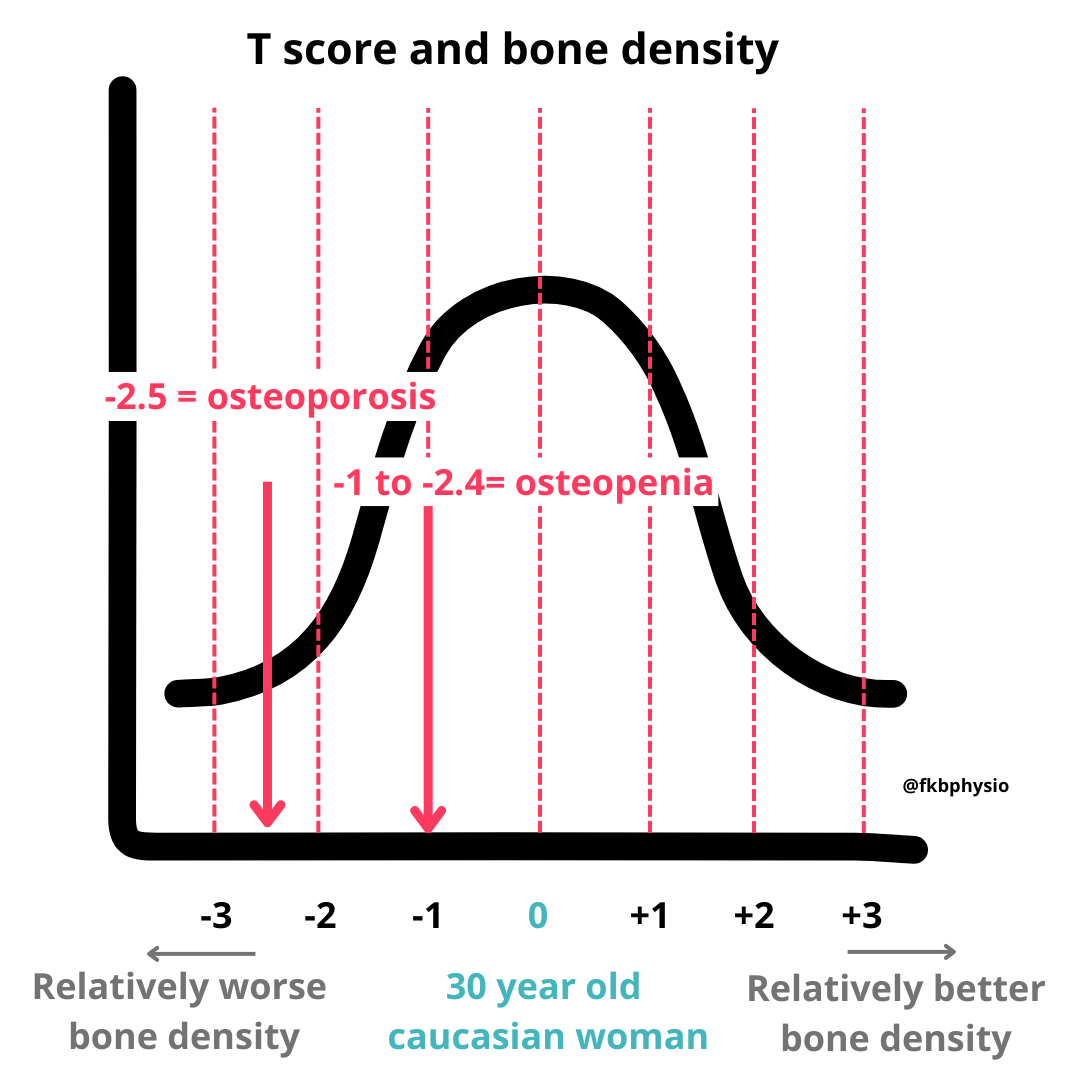
The official diagnosis according to the WHO is made based on your T score, which is a measure of your bone density relative to an average healthy 30 year old person of the same sex. This is calculated based on how many standard deviations you are away from that person. If you are more than 2.5 standard deviations away from the 30 year old, you are considered to have osteoporosis. Being between 1 and 2.4 standard deviations away is osteopenia. Any better than this is considered normal.
For people under 50, a T score is not used, rather a Z score is used which shows how far you are away from other people of your age and gender (Beck et al., 2017). This is likely because a T score is unlikely to be as sensitive at younger ages, that is, less able to detect an issue comparing to younger person so is more accurate comparing to your peers. Sometimes, on your scan you may see both the T and Z score. For example, I have had a patient in her 80s who had a T score of -1.2 that only just saw her into osteopenic range, which actually placed her above normal for her age, as seen with her Z score, which was +0.5. All of this is to say that these numbers are relevant, but are all recorded as relative values rather than set figures to aim for.
Osteoporosis is SILENT
Osteoporosis is silent, in that it has NO symptoms. A lot of people don’t know they have it until they have had a fracture, either from a fall, or from what is known as a “low trauma incident”, such as falling from standing height, or stepping down hard from a curb. There is no ache in the bones or joints, and no indication that you can feel that your bone density is low. I think this is an important point to make as patients often do not know this and believe that if they do not have pain, their bone density must be fine, and as such are not aware it may be something they should be checking. I always make sure to go through the difference between osteoporosis and osteoarthritis with my clients when they have a diagnosis of either.
Diagnosis is made by DEXA, but DXA is not perfect
DEXA scans are the current gold standard for bone density checks, however, there are issues with their accuracy.
There are DEXA Scans that look at whole body bone density, but it is particularly important to look at the bone density of the lumbar spine and hips as they often show lower scores, earlier, and as such are more sensitive to detect a decreasing density. Using whole body T scores is likely to underdiagnose osteoporosis or osteopenia (Rajaei et al., 2016).
DEXA scans are known to be relatively inaccurate. You are advised to get their scan at the same place every time. There are inaccuracies between pieces of equipment, brands, and also from practitioner technique. Going to the same clinic has the best chance at being accurate, and even then, a clinically significant difference is considered to be 4% change in bone density or more, anything less can be put down to measurement error.
A DEXA scan is also only a part of the story. The actual architectural structure of the bone is also important, a feature which is not represented by your typical bone density scan. Belinda Beck warns in her 2022 article that a DEXA does take into account all aspects of bone health such as cortical thickness of the bone. It is thought that BMD accounts for only 60% of the actual profile of bone fragility as it cannot measure changes in structure or bone material composition (Osterhoff et al., 2016). There are also certain conditions such as severe osteoarthritis can also affect the accuracy of the scan. Osteoarthritis makes T scores higher due to the additional bone that is a feature of the condition. So it is common to see people with a high T score in their spine but a very low T score in their hips, which is often more likely that their spine is osteoarthritic rather than that their hips are substantially worse.
Just a personal anecdote, my patients who have had low trauma fractures from have at times been women in their 50s with osteopenia, yet a lot of my clients in their 60s and 70s with osteoporosis have never had them. This is indicative of the DEXA scan being able to tell us one thing (BMD/T score) but not the whole story (bone architecture and general strength otherwise).
Despite these flaws, DEXA scans are a worthwhile screening tool to capture people whose bone health is declining, which is important as earlier detection allows for earlier interventions.
Management of osteoporosis
Everyone with osteopenia or osteoporosis is managed a little bit differently because everyone’s case is different. For example, a fit 60 year old with osteoporosis may be managed differently to a more frail 80 year old who has had a number of falls. This is particularly true when it comes to medical management of the condition.
There are a number of medications available on the market for osteoporosis, some which work to reduce the activity of bone break down, and others which work to increase the regeneration of new bone. Some names you may have heard are prolea or zolendronic acid, or the word bisphosphonates. There are newer ones coming out all the time. There are some reasons for and against medication that mean not every person with osteoporosis will be advised to start them straight away. There is somewhat limited data on the effect of the medications in the longer term (more than 10 years) (Hinton et al., 2015). Medication can be quite effective at reducing fracture risk, with some studies stating they can reduce fracture risk by up to 40% in the hip and 70% in the spine (Hinton et al., 2015). There are a number of potential side effects that are brought up and this is entirely a conversation to be had between a patient and their doctor.
Vitamin D and calcium are also important in the management of this condition and once again a conversation of whether to supplement these or not is something that is considered on an individual basis and is not within my or our scope to discuss. I will say that the guidelines set by osteoporosis Australia do not recommend supplementing vitamin D or calcium for people without diagnosed deficiencies, however, this is different to guidelines in other countries. It is best to consult with your GP about your specific situation.
The Canadian guidelines have a flow chart that is really useful to look at when considering the potential benefit of medication in the management of osteoporosis - you can check them out here and scroll down to page 4.
Lifestyle changes to reduce risk
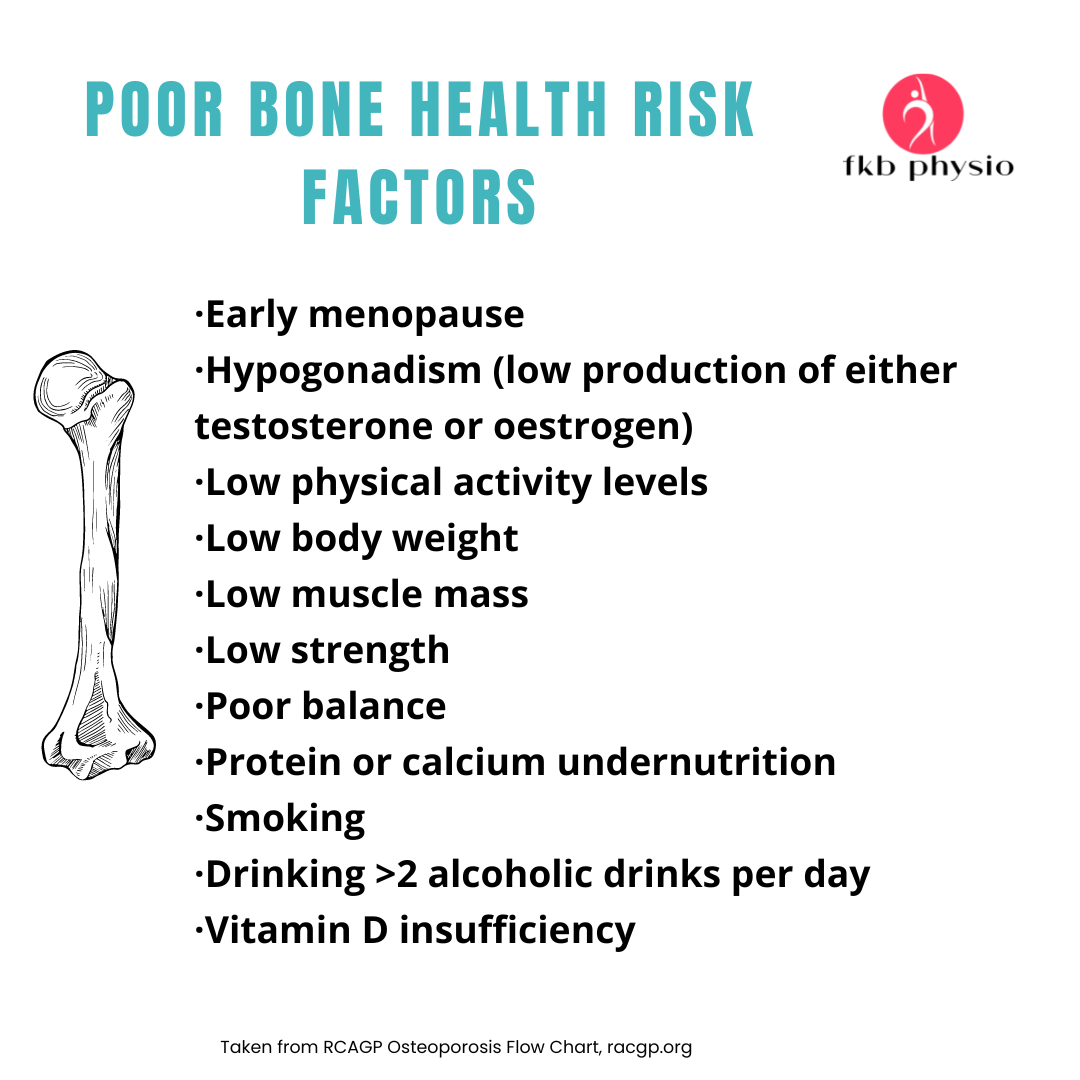
There are lifestyle modifications that promote bone health. Osteoporosis Australia has released a set of guidelines that apply to post -menopausal women and men over 50:
- Adequate calcium and protein intake
- 1300mg a day of calcium and 1g per kg of body weight of protein (this is A LOT of calcium - could be worth tracking your intake for a day and seeing how close you get)
- Adequate but safe exposure to sunlight as a source of vitamin D
- Avoid smoking and excessive alcohol consumption (considered more than 2-3 drinks a day)
- Participate in progressive resistance training and balance training exercise 2-3 days. Per week, moderate to vigorous, varied, and designed to reduce fracture and falls risk, as well as treat sarcopenia.
Exercise in the management of osteoporosis
All osteoporosis guidelines that I have come across recommend exercise as a pillar of bone health management, not just to improve bone density but also to reduce falls risk.
I believe that all adults who have the means to do so would benefit greatly from resistance training. If you have a bone density concern, it is really important to consult a healthcare professional who specialises in the area to help guide you towards a safe and effective program. If you don’t have any bone density concerns that you know of and are otherwise fairly fit and healthy, taking up strength training is probably one of the best things you can do. It is never too late to start, but the earlier you start the better!
If you want more specific information about exercise to manage osteoporosis, check out this blog post (coming soon!)
References:
1. Beck, B. R., Daly, R. M., Singh, M. A., & Taaffe, D. R. (2017). Exercise and Sports Science Australia (ESSA) position statement on exercise prescription for the prevention and management of osteoporosis. J Sci Med Sport, 20(5), 438-445. https://doi.org/10.1016/j.jsams.2016.10.001