Having a disc bulge is not as scary as you think
" I hope I haven't done a disc!!!"
The most common thing I hear when I see a client with a painful lower back is, ‘I’m really worried I’ve done a disc’.
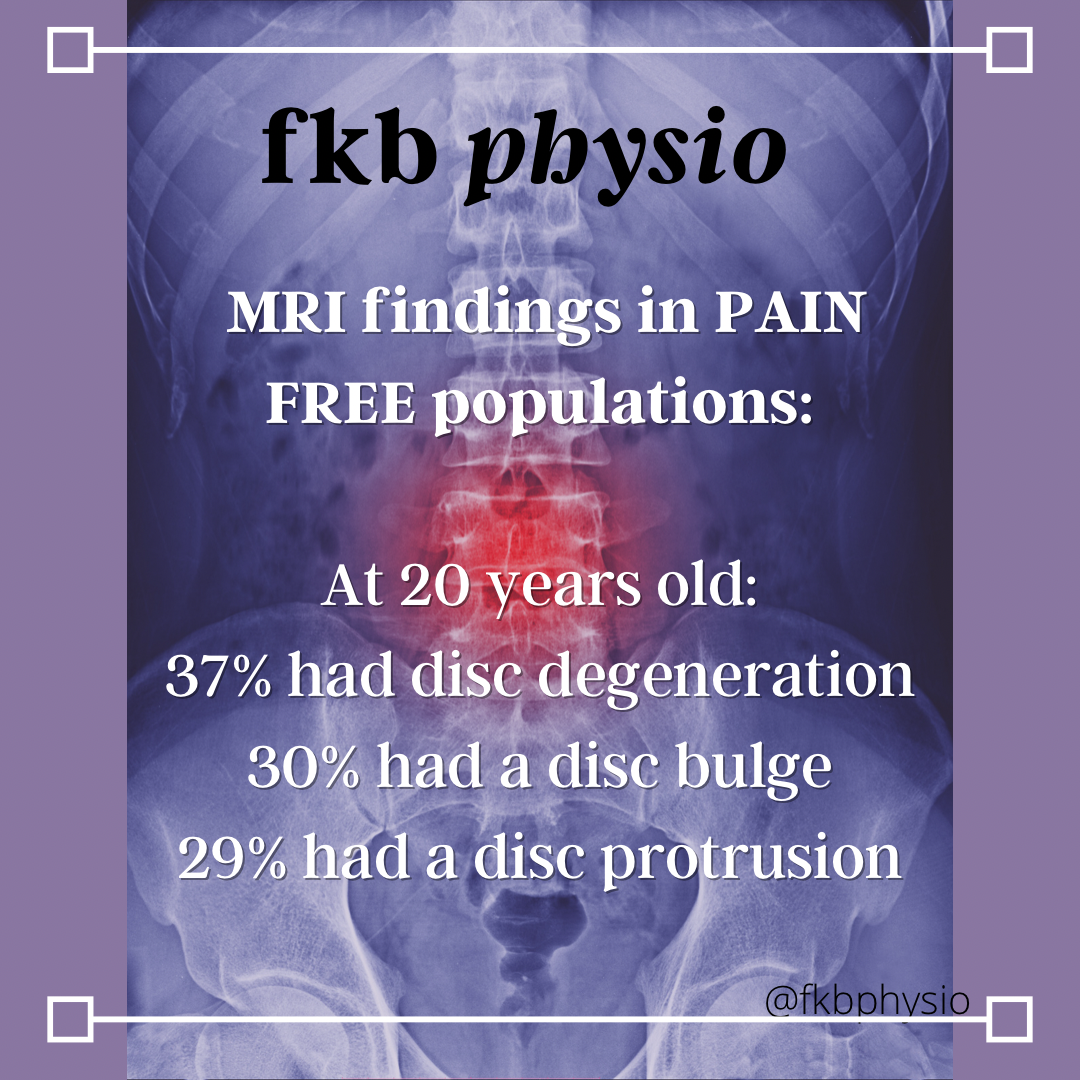
The idea of a disc bulge or herniation being correlated with a terrible injury is one of the most pervasive fallacies in the musculoskeletal realm, considering up to 50% of people aged 30-39 who have NEVER had low back pain have a disc bulge or herniation on imaging (Brinjikji et al., 2014). This number increases every decade.
In fact, there is evidence to show that people who receive an MRI early after feeling low back pain have a WORSE outcome and end up spending MORE money than those who don’t (Webster et al., 2013). This is potentially because being shown a disc injury on MRI is scary and worrying. It is often combined with being told that you have ‘slipped your disc’, and being advised that this can require surgery or lead to life long problems, which can cause the negative decline in function and self worth.
MRIs do have a place in the management of low back pain, and this role is to rule out sinister pathology. There are very rare instances in which there is an emergency that requires medical attention and in these cases an MRI is necessary to bring it up; however, there are specific red flags that indicate this is required. In the absence of red flags, it is NOT best medical advice to receive a scan. This is supported in the UK’s National Institute for Health and Care Guidelines regarding low back pain best practice management. It is not simply my opinion!
Your ‘diagnosis’ does not define your presentation
Someone with multiple disc bulges all through their lower back can be perfectly pain free, deadlifting heavy, and doing as they please. Someone with no disc injuries can be unable to cough, sneeze, or bend forward without pain. Whether or not you have ‘disc-like’ symptoms is unlikely to be related to the findings on your MRI.
The idea that a disc injury is lifelong, leads to problems later life, needs to be treated extra carefully, requires avoidance of heavy lifting and running, is INCORRECT. While there may need to be modifications made in the short term to aid someone to feel better, there is no reason this needs to spiral out into a long term problem.
Acute low back pain is PAINFUL and feels TERRIFYING
The reason this whole situation is so common with low back pain in particular is because low back pain is PAINFUL. The true 10/10 pains I have seen in my career have been those poor people bent over and hobbling in as a result of their sudden onset lower back pain. I have had it myself. The stereotypical ‘pop’ with instant severe pain across my back so bad I nearly passed out, with leg pain and pins and needles in the weeks following.
And it took all my mental energy to reassure myself that what I was going through felt MUCH worse than what it really was!
It is very easy to understand why someone with 10/10 pain walks into their GP’s office crying, and walks out with an MRI and a fear that they are ‘broken’. However, this pain is usually because of the inflammation associated with low back pain (and probably all those other things that affect our experience of pain listed earlier). Most of the time, once the inflammation has gone, the severe, acute pain is much less.
I understand it can feel negligent to not have a scan when they are in such pain, however in the VAST majority of cases, you will get an MRI and be told to ‘wait and see’ if your pain gets better. If it isn’t better in a set timeframe, then more treatment may be warranted. This ‘wait and see’ approach is likely to happen whether you get the MRI or not. The scan does not change the treatment path in the acute phase of low back pain. Considering MRIs are expensive, and associated with worse outcomes, and don’t actually change the treatment in the short term, it doesn’t make sense to get one in those first few weeks of low back pain, in the absence of any red flags.
So what can you do?
With an acute episode of low back pain, understanding that it is scary but probably not dangerous, and knowing that you are likely to feel better within 6 weeks can be reassuring. Finding a healthcare practitioner (physio or exercise physiologist) who will guide you through movements that you feel safe to do is probably your best option. Often, people rest completely while they are recovering and then find they keep re-hurting themselves when they try to get back to regular activities. Everyone needs a different level of support, but don’t feel afraid to reach out and find someone who can help.
I offer online consults as well as in person in Brisbane, Australia. Please don’t hesitate to get in touch!
Also, check out an upcoming blog “exercises for acute low back pain” for some movement ideas, but remember tailored exercises are always best.
References:
- Brinjikji, W., Luetmer, P. H., Comstock, B., Bresnahan, B. W., Chen, L. E., Deyo, R. A.,. Jarvik, J. G. (2015). Systematic literature review of imaging features of spinal degeneration in asymptomatic populations. AJNR. American journal of neuroradiology, 36(4), 811-816. doi:10.3174/ajnr.A4173
- Merskey H, Bogduk N. Classification of chronic pain, IASP Task Force on Taxonomy. IASP Press; Seattle: 1994
- NICE (2020), https://www.nice.org.uk/guidance/ng59/resources/low-back-pain-and-sciatica-in-over-16s-assessment-and-management-pdf-1837521693637
- Webster, B. S., Bauer, A. Z., Choi, Y., Cifuentes, M., & Pransky, G. S. (2013). Iatrogenic consequences of early magnetic resonance imaging in acute, work-related, disabling low back pain. Spine, 38(22), 1939-1946. doi:10.1097/BRS.0b013e3182a42eb6

